What is Pelvic Organ Prolapse?
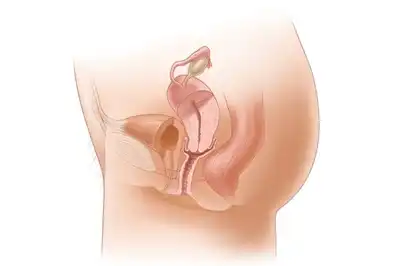
Pelvic Organ Prolapse is a condition in which one or more pelvic organs slip down from their normal position and bulge into the vagina due to weakness of the pelvic floor muscles and supporting tissues. The pelvic organs include the uterus, bladder, rectum, and vaginal walls.
In simple words, when the muscles and ligaments that support pelvic organs become weak or damaged, the organs lose support and begin to descend. This can cause discomfort, pressure, urinary or bowel problems, and difficulty in daily activities.
Pelvic organ prolapse is common but often under-reported, especially among women, because many feel embarrassed to talk about their symptoms.
Which organs are affected in Pelvic Organ Prolapse?
Depending on the organ involved, pelvic organ prolapse may include:
- Uterine prolapse – the uterus slips downward
- Cystocele – bladder bulges into the vaginal wall
- Rectocele – rectum bulges into the vagina
- Enterocele – small intestine pushes down
- Vaginal vault prolapse – the top of the vagina drops (after hysterectomy)
A woman may have one or multiple types at the same time.
Why does Pelvic Organ Prolapse occur?
Pelvic organ prolapse develops due to weakening or damage of the pelvic floor muscles and connective tissues.
Common Causes Include
- Pregnancy and normal childbirth
- Multiple or difficult deliveries
- Aging and muscle weakening
- Menopause and low estrogen levels
- Chronic constipation and straining
- Obesity
- Heavy lifting
- Chronic coughing
- Previous pelvic surgery
- Genetic weakness of connective tissues
Over time, these factors reduce pelvic support and lead to prolapse.
Who is at risk of Pelvic Organ Prolapse?
Women are more commonly affected, especially those who:
- Have given birth multiple times
- Had prolonged or difficult labour
- Are postmenopausal
- Are overweight
- Have chronic constipation
- Perform heavy physical work
However, pelvic organ prolapse can also occur in younger women and rarely in men (after pelvic surgery).
Types of Pelvic Organ Prolapse (By Severity)
Pelvic organ prolapse is graded based on how far the organ has descended.
Mild Prolapse
- Organs drop slightly
- Symptoms may be minimal
Moderate Prolapse
- Organs reach the vaginal opening
- Symptoms become noticeable
Severe Prolapse
- Organs protrude outside the vagina
- Daily activities become difficult
Early stages are easier to manage than advanced prolapse.
Common Symptoms of Pelvic Organ Prolapse
Symptoms vary depending on the organ involved and severity.
Pelvic Symptoms
- Feeling of heaviness or pressure in the pelvis
- Sensation of something coming down
- Visible bulge in the vagina
- Lower back pain
Urinary Symptoms
- Frequent urination
- Difficulty emptying the bladder
- Urine leakage
- Recurrent urinary infections
Bowel Symptoms
- Constipation
- Difficulty passing stools
- Feeling of incomplete bowel emptying
Sexual Symptoms
- Discomfort or pain during intercourse
- Reduced sexual satisfaction
Symptoms often worsen after standing for long hours or at the end of the day.
How does Pelvic Organ Prolapse affect daily life?
Pelvic organ prolapse can affect quality of life by causing:
- Physical discomfort
- Difficulty walking or sitting
- Emotional stress and embarrassment
- Reduced confidence
- Avoidance of social activities
Many women delay treatment due to a lack of awareness or fear of surgery.
Is Pelvic Organ Prolapse serious?
Pelvic organ prolapse is not life-threatening, but if left untreated, it can lead to complications such as:
- Chronic urinary infections
- Urinary retention
- Bowel dysfunction
- Worsening prolapse
- Ulceration of protruding tissues
Early care helps prevent progression.
How is Pelvic Organ Prolapse diagnosed?
Diagnosis usually involves:
- Detailed medical history
- Pelvic examination
- Assessment during coughing or straining
- Imaging tests (if required)
Diagnosis helps identify the type and stage of prolapse.
Conventional Medical Management of Pelvic Organ Prolapse
Treatment depends on age, severity, symptoms, and future pregnancy plans.
Non-Surgical Management
- Pelvic floor exercises
- Vaginal pessary
- Lifestyle modifications
Surgical Treatment
Surgery may be recommended in severe cases or when symptoms significantly affect daily life.
However, surgery may not be suitable for everyone and carries risks.
Role of Lifestyle in Pelvic Organ Prolapse
Lifestyle changes play a crucial role in managing prolapse.
Helpful measures include:
- Avoiding heavy lifting
- Managing constipation
- Maintaining a healthy weight
- Practising pelvic floor exercises
- Avoiding prolonged standing
These steps help reduce pressure on pelvic organs.
Homeopathic Treatment for Pelvic Organ Prolapse in Lucknow
Homeopathy offers a gentle, holistic, and supportive approach in managing pelvic organ prolapse, especially in early to moderate stages, elderly women, and during post-surgical recovery.
Homeopathic care focuses on:
- Strengthening pelvic floor muscles
- Improving tissue tone
- Reducing pelvic heaviness
- Managing urinary and bowel symptoms
- Supporting hormonal balance
- Improving overall vitality
Treatment is individualised, based on:
- Type and severity of prolapse
- Age and hormonal status
- Bowel and bladder habits
- Physical and emotional condition
Common Homeopathic Medicines Used
(Prescribed only after proper medical evaluation)
- Sepia – Uterine prolapse with pelvic heaviness
- Lilium Tigrinum – Dragging sensation and pelvic pressure
- Calcarea Carbonica – Muscle weakness and obesity-related prolapse
- Helonias – Pelvic weakness and fatigue
- Podophyllum – Rectocele with bowel symptoms
Benefits of Homeopathic Treatment
- Natural and non-toxic
- Safe for long-term use
- Helps slow progression
- Improves pelvic muscle tone
- Reduces discomfort
- Enhances quality of life
Pelvic Floor Exercises and Prolapse
Pelvic floor exercises help strengthen muscles that support pelvic organs. Regular practice under guidance can:
- Reduce symptoms
- Improve bladder and bowel control
- Prevent worsening
Exercises should be done correctly to avoid strain.
Pelvic Organ Prolapse after Menopause
After menopause, reduced estrogen weakens pelvic tissues, increasing prolapse risk. Supportive care focusing on muscle strength, nutrition, and hormonal balance is especially important during this stage.
Emotional Impact of Pelvic Organ Prolapse
Women with prolapse may experience:
- Anxiety
- Depression
- Loss of self-esteem
- Relationship stress
Emotional support, counselling, and reassurance are important parts of care.
Can Pelvic Organ Prolapse be prevented?
Many cases can be prevented or delayed by:
- Strengthening pelvic floor muscles
- Managing constipation early
- Maintaining a healthy weight
- Avoiding excessive strain
- Seeking early medical advice
Frequently Asked Questions
Is pelvic organ prolapse curable without surgery?
Early stages can often be managed without surgery.
Does pelvic organ prolapse worsen over time?
It may progress if untreated, but proper care can slow it.
Can young women get pelvic organ prolapse?
Yes, especially after childbirth or heavy strain.
Is homeopathy safe for pelvic organ prolapse?
Yes, as supportive care under expert supervision.
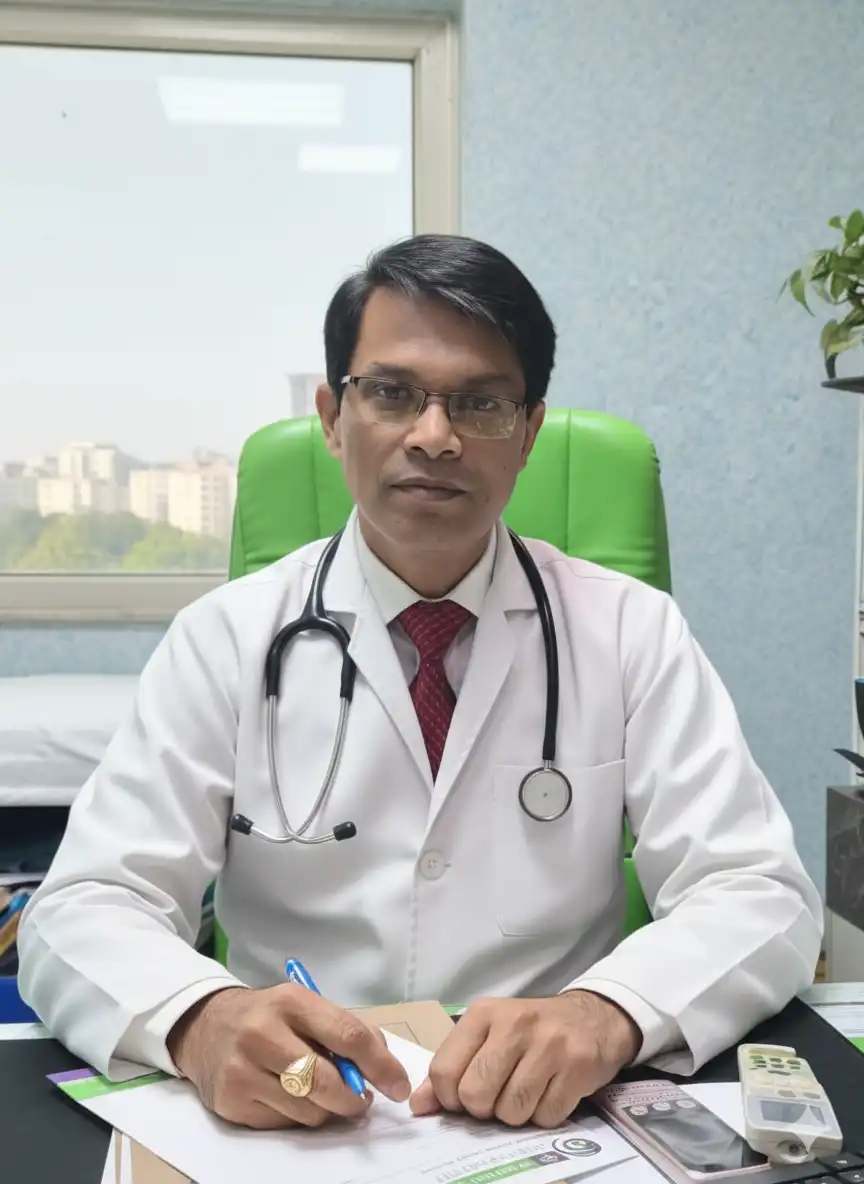
Why choose Dr. Sanjay’s Homoeopathy for Pelvic Organ Prolapse Treatment in Lucknow, India?
Dr. Sanjay’s Homoeopathy is a trusted clinic for safe and effective Pelvic Organ Prolapse treatment in Lucknow, India. With more than 22 years of experience, Dr. Sanjay Singh, MD (Homoeopathy), provides specialized homeopathy treatment that helps manage pelvic heaviness, bulging sensation, urinary or bowel difficulties, lower back pain, and discomfort during daily activities naturally without side effects. As a leading homeopathic doctor in Lucknow, he follows international treatment standards and offers a personalized approach that focuses on strengthening pelvic support structures, improving muscle tone, relieving symptoms, and preventing progression, making him the best homeopathy doctor for Pelvic Organ Prolapse in Lucknow. Patients from across India and around the world choose Dr. Sanjay’s Homoeopathy for its holistic healing, long-lasting relief, and compassionate care in managing women’s pelvic health conditions like Pelvic Organ Prolapse.